Wellness Insights
- Home
- Wellness Insights
- Human Papillomavirus Infection and Its Associated Risks
2022.03.25
Wellness InsightsHuman Papillomavirus Infection and Its Risks
Pharmacist Kuo, Kuo-Hua (Former Professor, Kaohsiung Medical University)
Human papillomavirus (HPV) is primarily transmitted through sexual contact. Studies have confirmed that HPV infection is the main cause of cervical cancer in women, accounting for approximately 2% of cancer cases in developed countries and 7% in developing countries. In the United States, about 70 million people are infected with HPV, with around 14 million new cases each year, leading to approximately 500,000 cases of cervical cancer and more than 250,000 deaths annually.
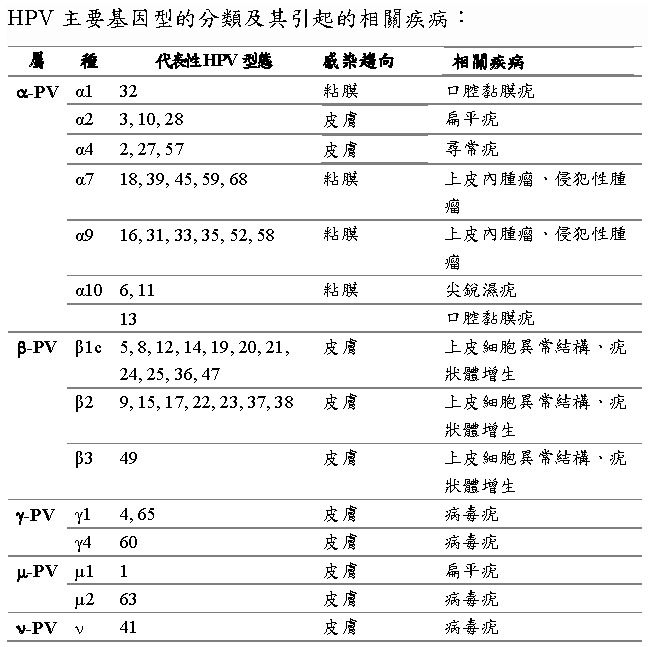
HPV can be classified into high-risk and low-risk types. High-risk HPV (such as type 16) is the primary cause of cervical cancer and is also strongly associated with other genital cancers in men and women, as well as head and neck cancers (oral, pharyngeal, esophageal, and tongue cancers). Most infections are “multitype infections,” and cannot be distinguished by appearance. Therefore, the goal of treatment should focus on complete elimination of the virus.
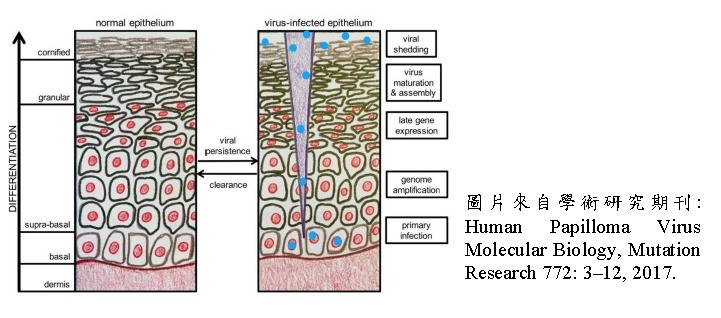
Patients should not rely solely on liquid nitrogen cryotherapy to remove visible lesions such as genital warts, as this only treats the surface and may overlook deeper viral infection that continues to pose a cancer risk. As shown in the figure below, HPV first infects the basal cell layer and gradually spreads upward to the epithelium, causing genetic abnormalities, cellular overgrowth, and continuous viral replication.
Based on the nature of the lesions they cause, HPV types can be divided into:
- Low-risk types: such as HPV6 and HPV11, which commonly cause genital warts (condyloma acuminata) or oral epithelial warts.
- High-risk types: such as HPV16 and HPV18, which lead to intraepithelial neoplasia that may progress to invasive cancer.
Approximately 5.2% of cancers worldwide are associated with high-risk HPV infection. Almost all cervical cancers are caused by HPV16 and HPV18. In addition, 95% of anal cancers, 70% of oropharyngeal cancers, 60% of vaginal cancers, 50% of vulvar cancers, and 35% of penile cancers are related to HPV infection.
Therefore, preventing HPV infection is extremely important, particularly for individuals with weakened immunity, organ transplant recipients, or those infected with HIV. These individuals have a significantly higher risk of cancer from both low-risk and high-risk HPV infections.
Current Status of HPV Prevention and Treatment
Since 2006, vaccination has been the only effective method to prevent HPV infection. Gardasil® was the first approved HPV vaccine in the world and protects against both low-risk types (HPV6, HPV11) and high-risk types (HPV16, HPV18). Cervarix® is a bivalent vaccine targeting HPV16 and HPV18. In 2014, the U.S. FDA approved Gardasil 9®, which protects against nine HPV types (HPV16, 18, 6, 11, 31, 33, 45, 52, 58).
According to the Advisory Committee on Immunization Practices (ACIP), all three vaccines may be used for routine vaccination of adolescents aged 11–12. Vaccination is also recommended for females aged 13–26, males aged 13–21 (and up to 26 for men who have sex with men), as well as individuals with weakened immunity.
It is important to note that HPV vaccines provide only prevention and do not treat existing infections. They also do not cover all HPV types. Even with widespread vaccination, the incidence of head and neck cancers caused by high-risk HPV continues to rise.
Once infected with HPV, clinical treatment mainly involves liquid nitrogen cryotherapy to remove visible lesions. This process is painful and cannot eliminate hidden viruses, leading to frequent recurrence. Currently, there are no oral treatment medications; topical creams have strong side effects and may cause secondary damage when widely applied.
Therefore, treatment should combine cryotherapy with restorative topical products to thoroughly eliminate residual viral cells and latent lesions, preventing recurrence and reinfection. Additionally, for individuals over age 26 or those who are sexually active, using moisturizing and lubricating topical preventive products can provide protection and comfort during sexual activity—especially beneficial for postmenopausal women.
The keys to preventing HPV infection include early vaccination, regular screenings, and safe sexual practices. DEING Bio continues to promote health education and prevention awareness to safeguard public health.
